WHO Report Warns Global Health Inequities Deepening Due to Social Injustice, Discrimination, and Poverty.
Geneva:
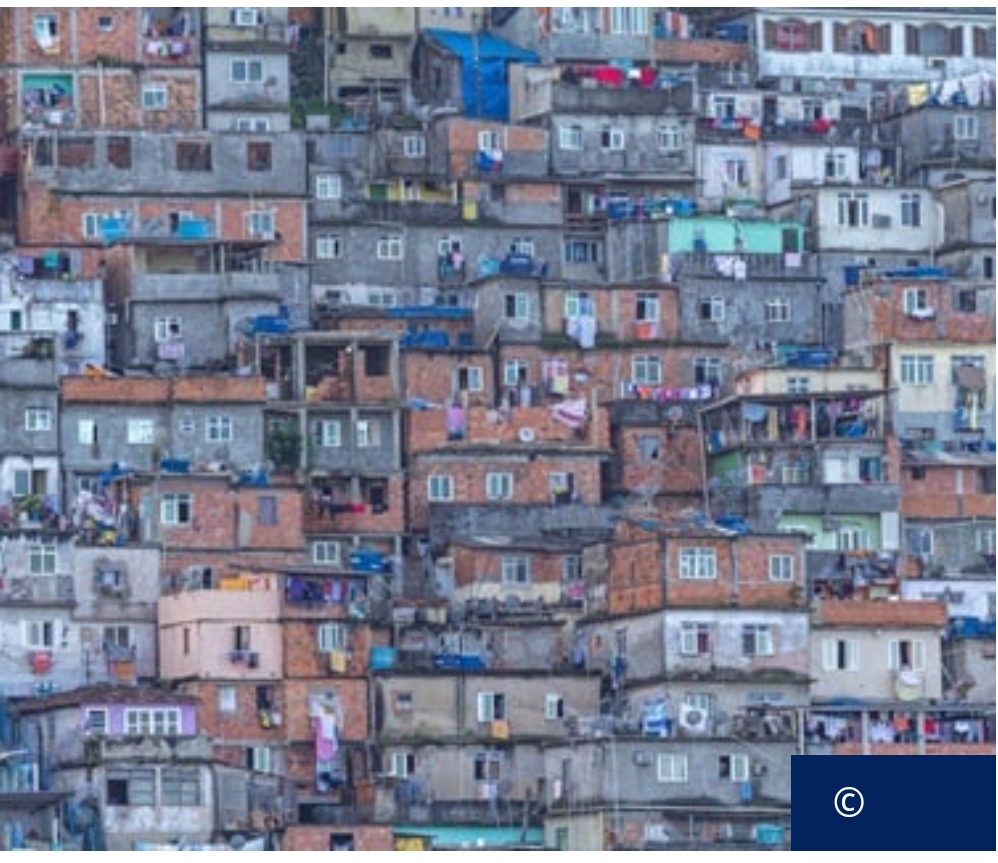
A landmark global report released by the World Health Organization (WHO) has raised alarm over the widening health disparities driven by deep-rooted social injustices, revealing that where a person is born, lives, works, and ages has a greater impact on their health than access to health care or genetics.
The World Report on Social Determinants of Health Equity, the first of its kind since 2008, presents stark evidence that inequities in housing, education, employment, and access to basic social protection are shortening lives—sometimes by decades—even in high-income nations. The report finds that people born in the country with the lowest life expectancy live, on average, 33 years less than those in the highest-ranking country.
“Our world is an unequal one,” said WHO Director-General Dr. Tedros Adhanom Ghebreyesus. “But change for the better is possible. This world report illustrates the importance of addressing the interlinked social determinants and provides evidence-based strategies and policy recommendations to help countries improve health outcomes for all.”
Poverty, Discrimination, and Marginalization at the Core of Health Disparities
The WHO report identifies that health follows a social gradient: the more disadvantaged people are socially and economically, the poorer their health outcomes and the shorter their healthy life expectancy. In marginalized populations such as Indigenous Peoples, both in wealthy and developing countries, this gap is particularly stark. Indigenous communities, for example, consistently have lower life expectancies and poorer maternal health outcomes.
Children born in low-income countries are 13 times more likely to die before the age of five than their peers in wealthier nations. WHO modeling indicates that 1.8 million children’s lives could be saved annually if countries closed the equity gap between the richest and poorest sectors within their populations.
Women from Disadvantaged Groups at Higher Risk
The report highlights persistent inequities in maternal mortality, noting that while global maternal deaths fell by 40% between 2000 and 2023, 94% of maternal deaths still occur in low- and lower-middle-income countries. Disadvantaged women, especially from marginalized racial and ethnic groups, are far more likely to die due to pregnancy-related complications. In some high-income regions, Indigenous women are up to three times more likely to die during childbirth compared to non-Indigenous women.
Gender inequality—including practices like child marriage—further compounds maternal health risks. The report emphasizes that empowering women and addressing gender disparities are essential steps toward improving global health outcomes.
Climate Change, Conflict, and Debt Are Exacerbating Inequities
Beyond income and discrimination, climate change, conflict, and economic instability are accelerating health inequities. The report warns that climate change may push 68 to 135 million more people into extreme poverty within the next five years, heightening vulnerability to poor health outcomes.
Additionally, 3.8 billion people globally still lack adequate social protection such as paid sick leave or child support, placing them at higher risk of illness and financial hardship. Meanwhile, rising debt burdens are hampering governments’ ability to invest in public health infrastructure. The 75 poorest countries in the world have seen a fourfold increase in debt interest payments over the past decade, diverting critical funds from health and social services.
A Call to Collective Action
WHO urges governments, civil society, academia, the private sector, and local communities to collaborate urgently on structural reforms that prioritize health equity. The report calls for:
- Investment in universal public services such as education, housing, and health;
- Elimination of structural discrimination and the health impacts of conflict and forced migration;
- Sustainable climate action and equitable digital transformation policies; and
- Decentralized governance, empowering local communities to lead health equity initiatives.
WHO stresses that bold, inclusive policies and sustained political will are essential to breaking the cycle of poverty and poor health, especially if the world hopes to meet its 2040 health equity targets set out in the 2008 WHO Commission report.
“The time for action is now,” Dr. Tedros concluded. “We must dismantle the structural barriers that prevent billions from achieving their right to health and well-being.”